Why eating less and exercising more doesn’t always work for long-term weight loss
By Eirik Garnas
www.OrganicFitness.com
If there’s one thing we’ve learned from the numerous studies investigating the effects of calorie restriction and exercise on weight loss, it’s that people usually creep up towards their original body weight when they start eating to satiety again or ease up on their training regime.
Despite these poor long-term results, the notion that we just have to exercise more and eat less seems so intuitively right and is also so deeply rooted in people’s belief systems that few question its accuracy. Some folks even claim that calories are all that counts and that it really doesn’t matter what you eat as long as you reduce your energy intake.

While a subset of the population manages to stay relatively lean by doing some type of regular exercise and eating purely based on their energy and macronutrient needs, it’s clear that this doesn’t work for everyone. We’re losing the war against obesity, and it seems that the mantra to eat less and exercise more could be doing us more harm than good.
The laws of thermodynamics
There are two laws of thermodynamics that are especially relevant to body weight regulation; the first law basically states that the form of energy may change, but the total is always conserved, and the second law says that the entropy of an isolated system does not decrease.
When discussing body weight regulation it’s essential that we always adhere to these laws of thermodynamics, and recognize that the amount of energy that is contained in the body will increase if energy intake is higher than energy expenditure. This basic fact is well supported in the literature, and studies show that increased food energy supply is more than sufficient to explain the obesity epidemic (1,2). We essentially eat a lot more calories than before, and this steady rise in energy intake has driven the increases in body weight over the past several decades.
So, it’s well established that weight gain results from an imbalance between how much energy we consume and how much we expend. However, this basic fact doesn’t tell us anything about why we actually overeat.

A general belief seems to be that weight gain simply results from inactivity, poor self-control and gluttony, and the first law of thermodynamics is extrapolated to mean that we can just tell people who are overweight and obese to eat less and exercise more to permanently shed the fat. The problem with this analogy is that the human body isn’t a passive vehicle, but rather fights to maintain what it considers to be a balanced state.
If we look beyond the basic concept of calories in vs. calories out and start to dig a little deeper into human physiology and the scientific literature, it quickly becomes clear why deliberately restricting calories and exercising more isn’t an effective strategy for permanent weight loss for many individuals.
You’re fighting your brain’s hard-wired mechanisms for regulating fat storage
Have you ever wondered how some people maintain a relatively constant body weight year round, why an obese person over-consumes food even though he has plenty of stored energy in the form of body fat, or why restricting caloric intake doesn’t result in a linear decrease in fat mass depending on the magnitude of restriction?
The answers to these questions seem to lie in the intricate feedback system between the brain, gut, and fat cells…
The body fat setpoint and homeostatic regulation of body fat
In 1840, a doctor named B. Mohr was one of the first researchers to discover that obese people often have damage in certain areas of the brain. Since these first discoveries, we’ve learned that the hypothalamus in the brain is the primary control center for the system in our body that regulates fat storage on a long-term basis (the energy homeostasis system).
The amount of fat mass we carry is biologically regulated, and the brain tries to keep body fat within a certain range by influencing our appetite, body heat production, metabolic rate, and whether energy is directed towards fat tissue or lean mass. We essentially have a body fat setpoint that the brain homeostatically guards (3,4,5,6).
If we try to alter the amount of body fat we carry by manipulating food intake and physical activity induced energy expenditure, the brain will act to bring fat mass back to the original level by increasing hunger and decreasing energy output. Since these mechanisms can only prevent a certain degree of fat loss, we will naturally start to lose weight when we reduce the amount of calories we consume and/or exercise more. However, as most people who have restricted calories for some time know, we will also be hungry and tired.

As sustained voluntary calorie restriction significantly impacts the quality of life and requires a high level of discipline, most people eventually start to eat to satiety again and usually creep back up towards their original body weight.
A study published in the American Journal of Clinical Nutrition clearly illustrates the idea behind the body fat setpoint. They gave lean and overweight subjects a diet that contained 50% more calories than they naturally consumed, and as expected, all of the participants gained a significant amount of weight during the six weeks of overfeeding. The brain tried to defend the body fat setpoint by increasing metabolic rate and body heat production, but these compensatory mechanisms can only prevent a certain degree of fat gain. The interesting thing happened when the overfeeding phase was over and subjects were allowed to eat as much as they wanted for the following six weeks. All of the participants lost the majority of the weight they had gained although they didn’t restrict calories (7).
Calorie restricted dietary interventions point to the same thing; while deliberately reducing energy intake and increasing energy expenditure is necessary for someone who’s already lean and wants to lose more weight, it’s not a long-term strategy for those that are overweight and obese. What we have to do is acknowledge that weight loss isn’t just about making a conscious decision to eat less and exercise more.
The thermostat in your house is a good representation of how the homoestatic system works. If it’s cold outside and you open all the windows to your house, the heating system will kick in to try to keep the temperature around the adjusted setpoint (e.g., 72 degrees F). If you keep the windows open, the heating system will always try to get the temperature back up, but it can only compensate for some of the lost energy. However, if we close the windows, the temperature will quickly rise back to the original setpoint.
The same principles apply to homeostatic regulation of body fat. If we expend energy by exercising more or eating less, the brain will decrease metabolic rate, increase hunger, reduce body heat production, etc. in an attempt to fight fat loss. If we chronically restrict calories we will lose weight, but the body will always try to get things back to what it considers to be a balanced state. When we can no longer take the cravings and begin eating to fullness, our body weight creeps back up towards the original setpoint, and we get a feeling of defeat and failure.
The brain is less sensitive to signals from fat cells in people who are overweight and obese
If the energy homeostasis system was always working properly, no one would be obese. Why doesn’t the the brain respond to the elevated fat mass in people who are overweight by decreasing hunger and increasing metabolic rate, heat production, and use of stored fat as energy?
Part of the answer to this question is found in the negative feedback system between fat stores and the brain. Signaling hormones travel between fat cells and the control center in our head and enable the brain to measure and regulate the amount of body fat we carry.
The key hormone involved in this process is Leptin. Leptin is produced by the body’s fat stores which then travels to the brain where it produces a response at the receptors in the hypothalamus. A high leptin signal is supposed to ramp up the use of stored energy and trigger less interest in food, while a low leptin signal should initiate food seeking behaviour and energy conservation (3,5).
Since leptin production correlates with with the size of the fat stores, people who carry plenty of fat mass produce a lot more leptin than someone who is lean. So, why isn’t the brain responding to these high concentrations of circulating leptin by decreasing interest in food and burning more stored energy? Studies have made it clear that overweight and obesity are characterized by decreased leptin sensitivity, which means that the brain doesn’t respond adequately to the signal from leptin (5,8).
Let’s consider an example to illustrate the effects of leptin resistance on weight gain. Let’s say we have a woman who weighs 300 lbs. Although the fat stores of this person produce a substantial amount of leptin, the brain only responds partially to the signal and therefore thinks that the body carries less fat mass than it actually does. If the woman loses even more leptin sensitivity, the brain will trigger hunger and decreased energy expenditure in an attempt to store more fat and boost leptin production further.
So, it could seem that the more leptin resistant we become, the more body fat we have to carry to maintain the same level of leptin signaling in the brain. If we suddenly become very leptin resistant and the brain only receives half the signal from leptin (hypothetical), fat mass will double over time and we will settle in at a new, higher body fat setpoint.

This is not to say that leptin is the only factor involved in the feedback mechanism between fat cells and the brain, far from it. However, leptin signaling seems to be a key component and is also intuitively easy to grasp in the sense that leptin resistance is similar to a malfunctioning “thermostat”. While a lean person’s fat thermostat keeps body weight around a lean setpoint, the thermostat of someone who is obese is constantly elevated.
Leanness is the most natural state of the human body, and a perturbation of the energy homeostasis system results from a gene-environment mismatch
Have you ever considered the fact that humans and animals living in a specific ecological niche are relatively lean almost year round? Wild animals, hunter-gatherer tribes and some non-westernized populations all maintain a fairly low level of body fat, and increases in fat mass only happen when it’s appropriate for survival and reproduction (9,10,11). As I discussed in my last guest post at BretContreras.com, some traditional populations such as the Kitavans remain lean even though they have access to an abundance of food and are only moderately physically active. Studies also show that hunter-gatherers have leptin levels that are many times lower than westerners, indicating a well-functioning feedback system between fat cells and the brain (8,12).
While this doesn’t mean that we have to emulate the lifestyle of our paleolithic ancestors to be healthy, it does suggest that some aspects of our modern environment perturb the body’s mechanisms for regulating fat storage.
The key in figuring out why the body fat setpoint is elevated in overweight and obesity is to study non-industrial populations that are lean and healthy, and then use this information as a framework for deciphering the latest scientific research on homeostatic regulation of body fat. Only by removing the factors that cause the body to want to store more weight can we design an effective weight loss strategy.
So, how do I lower my body fat setpoint and lose weight?
While there’s still a lot we don’t know about the underlying causes of leptin resistance, elevated body mass setpoint and overeating, it’s clear that changes to the setpoint can be both a cause and consequence of weight gain, and that inflammation in the hypothalamus and food reward play an especially important role (3,5,13). That’s all well and good, but what we really need to know is how we can tweak our diet and lifestyle to lower the setpoint, eat less without deliberately restricting calories, and lose weight. Let’s briefly take a look at some of the practical solutions to long-term weight loss.
Avoid highly rewarding food
Numerous obesity researchers now consider food reward to be an essential factor in the modern obesity epidemic (3,4,14,15). The reward center in our brain labels things as good or bad and makes us seek out energy dense food, warmth, sex and other types of behaviours that benefit survival and reproduction in a natural environment.
The problem is that this system isn’t designed to handle Big Mac’s, donuts, cookies, and other western foods. These processed products are engineered to be addictive in the sense that they contain a wide spectrum of rewarding properties such as fat, starch, salt, sugar, and glutamate. And it’s not just the highly processed stuff that is problematic. Even salted nuts and deep-fried, cured bacon contain a fairly rewarding combination of fat and salt and probably shouldn’t make up a large part of your diet if your trying to lose weight.

So, what this basically means is that the energy homeostasis system evolved to deal with simple, whole foods such as meat, fresh fruits and vegetables, and that modern, processed foods alter the brain’s mechanisms for regulating fat storage. Studies suggest that leptin action in the brain is insufficient to inhibit overeating of highly processed food, because these rewarding products engage powerful neural responses that oppose leptin (5).
It’s really a vicious cycle where hyper-rewarding food triggers addictive processes in the brain and overeating. Energy imbalance leads to more fat mass, leptin resistance, and consequently a higher food intake (15).
Bottom line: Highly rewarding, processed food drives weight gain. A diet primarily composed of simple, whole foods should be the key component of any weight loss program.
Take good care of the trillions of microorganisms that live in and on your body
Besides food reward, all of the microbes that live in and on the human body (the human microbiome) seem to play an essential role in the whole process of inflammation, leptin resistance, and weight gain. In a guest post for BretContreras.com, I highlighted the fact that the human body is only 1% human from a genetic perspective and that the microbiome provides functions that stretch far beyond the physiological capabilities of the human host.
The bacteria living in the gastrointestinal tract (gut microbiota) are especially important to our overall health as they maintain healthy gut barrier function, digest otherwise indigestible food components, and regulate our immune system. The problem is that antibiotics, highly processed food, caesarean sections, and other factors associated with life in the modern world perturb the microbiome and promote a state of dysbiosis. The balance of “good” and “bad” microbes in the body has shifted, and the gut microbiota becomes inflammatory.
So, how is it that bacteria potentially can influence systemic inflammation, leptin sensitivity, and weight gain? One of the leading current hypotheses is that dysbiosis increases gut permeability and allows toxins found in the wall of proinflammatory bacteria to interact with our immune system and enter into systemic circulation. These endotoxins then trigger a state of low-grade chronic inflammation and leptin resistance in the hypothalamus (8,16).
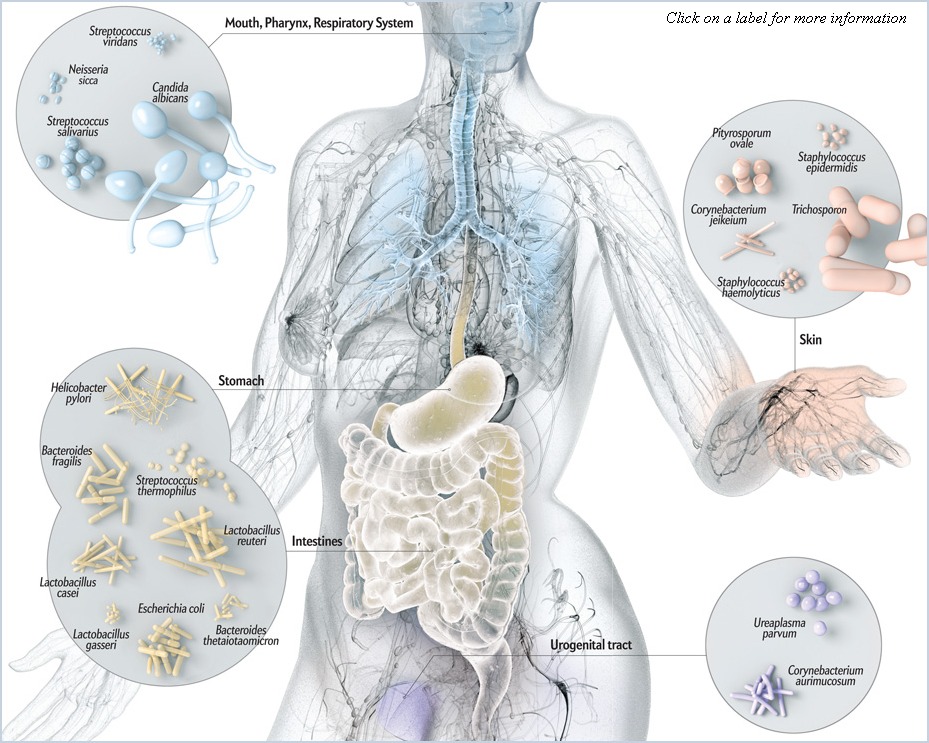
The human microbiome is one of the hottest topics in the scientific community at the moment, and numerous studies show that obesity is associated with changes to the gut microbiota (17,18). So, although the human microbiome is shaped throughout our life, it’s largely inherited from our family, and part of the hereditary component of obesity therefore results from transferring an “obese microbiota” from mother to child.
While more long-term human studies are needed before we know to which extent bacteria affect weight regulation, it’s already clear that the human microbiome has a profound impact on our health and well-being.
Bottom line: The human microbiome is involved in body fat regulation. Avoid antibiotics if possible, breastfeed your children, and preferably perform a vaginal birth. Avoid food that promotes the growth of harmful bacteria (e.g., highly processed food, refined flours, sugar), eat food that encourages the growth of beneficial bacteria (e.g., onions, leeks, properly prepared legumes), and eat “probiotics” (e.g., sauerkraut, kefir, dirty vegetables from the garden).
Exercise to improve metabolic health and build muscle
I know I’ve just made the case that exercising really isn’t effective for weight loss, but let’s look a little deeper. About a year ago I reviewed the scientific literature on exercise and weight regulation and concluded that isolated anaerobic or aerobic exercise usually isn’t very effective for weight loss. Most people compensate for the increased energy expenditure by eating more and/or being less active during the rest of the day, and exercising to “burn the fat” therefore makes little sense. This is also consistent with the body fat setpoint theory which suggests that the brain homeostatically guards a certain amount of fat mass.

However, some people respond to exercise by losing a fair amount of weight, and this probably has to do with the beneficial effects exercise has on metabolic health. A moderate amount of exercise has been shown to reduce inflammation and improve leptin and insulin sensitivity (19,20,21,22,23).
For the record, no one’s arguing that heavy resistance training and aerobic exercise aren’t an important part of a healthy lifestyle, it’s just that exercising to lose weight (and keep it off) isn’t effective for the vast majoity of people.
Bottom line: Exercising to “burn calories” makes little sense since most people compensate for the increased energy output by eating more food and/or being less active during the rest of the day. However, regular exercise allows you to eat more food without gaining weight and can also have a small impact on weight loss.
Make sure you’re eating enough protein
The Protein-Leverage Hypothesis suggests that humans aim for a targeted protein intake and that protein is prioritized over fat, carbohydrate, and total energy intake (24,25,26). A recent study also shows that body-weight loss and weight-maintenance on a low-carbohydrate diet seems to depend more on the protein consumption than the carbohydrate intake (27).

One common mistake among people who want to lose weight is to only eat foods such as fruits and vegetables in an attempt to reduce energy intake. While fruits and vegetables are great, they are also very low in protein and energy and should be matched with grass-fed meats, seafood, eggs or dairy to make for a more satiating meal. Eating carrots, cucumbers and tomatoes for breakfast and lunch won’t help your weight loss efforts since your body will crave for more energy and protein later in the day.
Bottom line: Protein is a very satiating macronutrient and should make up at least 15% of your daily energy intake.
Properly prepare whole grains, legumes and other plant foods that are difficult to digest
While everyone agrees that refined flours shouldn’t make up a large part of a healthy diet, some researchers have also speculated that the human leptin system isn’t adapted to a diet based on whole grains because antinutrients and proteins in cereal grains potentially contribute to leaky gut, inflammation, and leptin resistance (8,28,29). While some reports suggest that a grain-free diet is superior to a grain-based diet in terms of weight loss (8), few long-term human studies have found a causal link between consumption of grain fiber and weight gain.
Sensitivity to “toxins” found in grains seems to vary from person to person depending on human genetics, gut health, and whether we have the necessary microbial genes in the intestine to degrade harmful antinutrients and proteins. The problem seems to be that many people make cereal grains the staple of their diet and therefore eat less of more satiating foods such as fruits and vegetables (30).
The fact is that modern wheat is very different from the grains our ancestors used to eat. While celiac disease affects below 1% of the population, some studies suggest that gluten sensitivity is on the rise, and gluten and wheat germ agglutinin can be damaging even for those without celiac disease (31,32,33). A recent study also found that a gluten-free diet reduces adiposity, inflammation, and insulin resistance (34). Although several recent diet books make the case that gluten should be avoided by everyone, the fact is that few long-term human trials have investigated the effects of gluten on body weight regulation and health.

Healthy grain-based cultures usually soaked, grinded and/or fermented grains and legumes to make them more nutritious and easier to digest. Using these traditional processing techniques could be a viable option if you’re sensitive to antinutrients and/or eat a lot of legumes and cereal grains on a daily basis. Even just soaking oats overnight in water and lemon juice and then cooking over low-moderate heat will make for a healthier dish than just plain oats and milk.
Bottom line: Improperly prepared cereal grains are hard on the digestive system, but more research is needed to establish the exact role antinutrients and proteins such as gluten play in the modern obesity epidemic. Eating grains at the majority of your meals probably isn’t a good idea if you’re trying to lose weight, because grains contain some potential gut-irritating compounds and are typically lower in micronutrients and less satiating compared to fruits and vegetables. Traditional processing techniques make whole grains and legumes easier to digest.
Other strategies to lower inflammation and/or unconsciously reduce food intake
Several other factors such as insufficient sleep (35,36,37), high omega-6/omega-3 ratio (38,39,40), low vitamin D levels (41,42) and high cooking temperature (43,44,45) have also been associated with increased low-grade inflammation and/or obesity. While probably not as important as the major factors above, these things also play a role.
Putting it all together
Areas in the brain maintain the size of the fat stores within a certain range by influencing food intake and energy expenditure. In a “natural” environment, the energy homeostasis system regulates body weight at a level that is optimal for survival and reproduction, and leanness is therefore the natural state of Homo sapiens. Dysregulation of the energy homeostasis system and elevation of the body fat setpoint result from a gene-environment mismatch in the sense that the body’s mechanisms for regulating fat storage aren’t designed to handle highly rewarding food, broad-spectrum antibiotics, insufficient sleep on a long-term basis, and other factors associated with life in the modern world. If we try to lose weight by increasing exercise induced energy expenditure and/or restricting calories, areas in the brain that are responsible for regulating fat storage will trigger hunger and decreased energy expenditure in an attempt to regain the lost fat mass. To be able to design a plan that will cause permanent weight loss, we have to address the factors that are causing the body to want to store more weight. Only then can we ramp up the use of stored body fat and eat less without deliberately restricting calories.
I want to make it perfectly clear that deliberate calorie restriction is necessary if you are already relatively lean, but still want to lose more weight. The reason for this seems to be that very low fat mass is below what is considered optimal for survival and reproduction, and the brain therefore protects fat stores by increasing hunger and decreasing body heat production and metabolic rate. I also want to emphasise that although everyone can lose a substantial amount of weight if they adhere to the principles outlined in this post, genetics do matter.

Eat a diet primarily composed of simple, whole foods such as meat, seafood, eggs, vegetables, grass-fed dairy, fruits, nuts, and properly prepared whole grains and legumes. Make sure you get enough protein. Take care of the microbiome by eating prebiotics, beneficial bacteria, and avoiding food that encourages growth of harmful bacteria. Exercise to improve metabolic health, try to get enough sleep, make sure you’re getting enough vitamin D and omega-3, and reduce the production of advanced glycation end products by gently cooking your food.
Individual differences are important, and while some people are able to stay lean while still eating a fair amount of highly-processed food, others must make a significant effort to reduce the reward value of the diet, improve gut health, and follow all the other recommendations.
About the author
 Name: Eirik Garnas
Name: Eirik Garnas
Website: www.OrganicFitness.com
Besides studying for a degree in Public Nutrition, I’ve spent the last couple of years coaching people on their way to a healthier body and better physique. I’m educated as a personal trainer from the Norwegian School of Sport Sciences and also have additional courses in sales/coaching, kettlebells, body analysis, and functional rehabilitation. Subscribe to my website if you want to read more of my articles on fitness, nutrition, and health.
The post Why eating less and exercising more doesn’t always work for long-term weight loss appeared first on Bret Contreras.

Leave a comment